Platelet-Rich Plasma
Eclipse PRP® is a proprietary system that is based on blood separation according to density using a unique separation gel. The PRP platform is available with an 11 mL PRP collection tube or 22 mL high concentration collection tube. The system allows for the preparation of pure Platelet-Rich Plasma (PRP) with optimal platelet concentrations and cellular content. Virtually, all Red Blood Cells (RBC) are eliminated from PRP and the concentration of pro-inflammatory Granulocytes (GRs) is highly reduced.
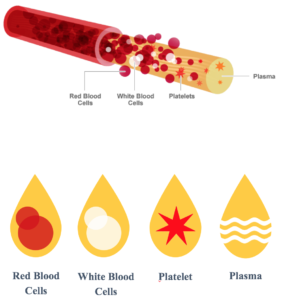 Platelet-Rich Plasma is prepared by taking a small sample of the patient’s own blood, then separating platelets from Platelet-Poor Plasma (PPP), RBC and GRs via centrifugation. Next, the PRP is collected and may be applied to the treated site. The whole preparation process only takes up to 20 minutes.
Platelet-Rich Plasma is prepared by taking a small sample of the patient’s own blood, then separating platelets from Platelet-Poor Plasma (PPP), RBC and GRs via centrifugation. Next, the PRP is collected and may be applied to the treated site. The whole preparation process only takes up to 20 minutes.
Upon activation, platelets release growth factors and other molecules. These growth factors are regeneration-promoting signaling molecules, such as Platelet-Derived Growth Factor (PDGF), Transforming Growth Factor group (TGF), Epidermal Growth Factor (EGF), Vascular Endothelial Growth Factor (VEGF), Fibroblast Growth Factor (FGF) and others. These molecules are shown to regulate the healing cascade, including inflammation and cell proliferation.
FAQ
Q: What is Platelet- Rich Plasma?
A: Autologous Platelet-Rich Plasma, also known as PRP, is a high concentration of your own platelets in a small volume of plasma.
Q: How long does the PRP process take?
A: The blood draw takes just a couple of minutes, followed immediately by a 10-minute centrifugation. The time involved in the application varies based on which procedure is being performed.

Q: How many PRP sessions are required?
A: Your medical professional can create a treatment plan based on your individual needs.
Q: Can a PRP procedure be painful?
A: Eclipse PRP® is close to a physiologic pH, which means the product is less likely to cause a stinging or burning sensation. There may be some temporary discomfort or possible redness and inflammation at the application site, but quickly resolves.
Q: Is PRP safe?
A: Since the autologous Platelet-Rich Plasma (PRP) is produced from a patient’s own blood, there is virtually no risk of an allergic reaction or rejection.

SAFETY INFORMATION
INTENDED USE
Safe and rapid preparation of autologous platelet-rich plasma (PRP) from a small sample of blood at the patient point of care. The PRP is mixed with autograft and/or allograft bone prior to application to a bony defect for improving handling characteristics.
PRECAUTIONS
- PRP should be applied to the same patient from whom the blood was drawn.
- Storage of tubes containing blood at or below 0°C may result in tube breakage.
- Storage of tubes above 40°C may damage the gel stability.
- Do not remove conventional rubber stoppers by rolling with a thumb. Remove stoppers with a twist and pull motion.
- Do not use tubes if foreign matter is present.
- All liquid preservatives and anticoagulants are clear. Do not use tubes after their expiration date.
- Do not re-sterilize and do not attempt to clean this product.
- Do not use products if pouch is damaged.
- Use prepared platelet concentrate material within 4 hours after drawing blood from patient.
CAUTION
- Practice Universal Precautions. Process all procedures under controlled environment, use gloves, gowns, eye protection, other personal protective equipment and engineering controls to protect from blood splatter, blood leakage and potential exposure to blood-borne pathogens.
- All glass has the potential for breakage. Examine all glass for potential damage in transit before use and take precautionary measures during handling.
- Handle all biologic samples and blood collection “sharps” (lancets, needles, luer adapters, and blood collection sets) according to the policies and procedures of your facility. Obtain appropriate medical attention in the event of any exposure to biologic samples (for example, through a puncture injury) since they may transmit viral hepatitis, HIV (AIDS), or other infectious diseases. Utilize any built-in used needle protector, if the blood collection device provides one. Estar Technologies Ltd. does not recommend reshielding used needles.
- Discard all blood collection “sharps” in biohazard containers approved for their disposal.
- Transferring a sample from a syringe to a tube is not recommended. Additional manipulation of sharps increases the potential for needlestick injury, in addition, depressing syringe plunger during transfer can create a positive pressure, forcefully displacing the stopper and sample and causing a potential blood exposure. Using a syringe for blood transfer may also cause over or underfilling of tubes, resulting in an incorrect blood-to-additive ratio and potentially incorrect analytic results. Tubes with draw volume smaller than the apparent indicated dimensions may not be filled to their stated volume when filled from a syringe. The laboratory should be consulted regarding the use of these samples.
- Underfilling of tubes will result in an incorrect blood-to-additive ratio and may lead to incorrect analytic results or poor product performance.
POSSIBLE SIDE EFFECTS
- Damage to blood vessels, hematoma, infection and/or irritation.
- Temporary or permanent nerve damage that may result in pain or numbness.
- As with any injection-based treatment, infection is a slight possibility.